There is growing attention to
providing culturally competent health care to our patients/families who are
lesbian, gay, bisexual or transgender (LGBT). This raises a few questions: Why
is this needed? What does LGBT culturally competent health care mean? How do we
go about achieving this? I hope to offer some insight into these basic
questions in this blog and to whet your appetite to learn more in a
Train-the-Trainer webinar that will occur in June 2016.
Let’s begin with a working definition of cultural competence. There are several definitions that have been
offered over the years. One of the seminal works in the field of “cultural
competence” dates to 1989 when Terry L. Cross, et al wrote Towards a Culturally Competent System of Care: A Monograph on Effective
Services for Minority Children Who Are Severely Emotionally Disturbed [Cross, Bazron, Dennis, and Isaacs
(1989)]. In it they describe cultural
competence as a “set of congruent behaviors, attitudes, and policies that come
together in a system, agency, or amongst professionals to work effectively in cross-cultural
situations.” In practice, “a culturally competent system of care acknowledges
and incorporates, at all levels, the importance of culture, the assessment of
cross-cultural relations, vigilance towards the dynamics that result from cultural differences, the expansion of
cultural knowledge, and the adaptation of services to meet culturally unique
needs”.
Why should we address LGBT cultural
competence in health care? It has been difficult to get a completely accurate picture of the health
disparities facing the LGBT communities because we don’t regularly collect
sexual orientation and gender identity data like we do for other demographic
groupings e.g., race, ethnicity and language. There have been a few relevant
studies conducted that help us understand the need for addressing this today in
the health care arena. In the 2007 California
Health Interview Survey we see the disparities between LGB populations and
the heterosexual population in seeking preventive care and in divergent use of
emergency services:
% adults delaying/not seeking health care
- Heterosexual
– 17%
- LGB
– 29%
% adults receiving
emergency health care
- Heterosexual
– 18%
- LGB
– 24%
In the study When Healthcare Isn’t Caring (2010, Lambda Legal’s Survey
on Discrimination Against LGBT People and People Living with HIV) we get a
picture of the “perception of care” from the perspective of these groups. 7.7%
of LGB and 26.7% of Transgender respondents report they were refused medical
care because of sexual orientation or gender identity. Given this it is not
unsurprising to see that some LGBT people have the perception that they will be
refused future health care for the same reason: nearly 10% of LGB and 52% of
Transgender respondents believe they will be refused health care.
Our work is to reduce health
disparities and to encourage people to get the health care needed in spite of
cultural differences whether sexual orientation, gender identity, or any other cultural
factor.
What does LGBT culturally competent health care mean? One of the leaders in advocacy for
LGBT people in receiving equality in health care is the Human Rights Campaign
Foundation which publishes the Healthcare Equality Index (HEI) each year. The HEI provides
a road map for healthcare systems in measuring best practices for LGBT patient
– and- family centered care and for LGBT workforce inclusion.
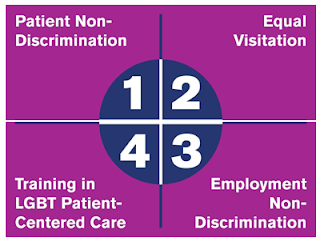
The Core Four Requirements of the HEI
address the following four broad policy and procedure areas for health care
facilities:
In addition the self-reported survey
assesses best practices and gives concrete examples for practices in the
following areas:
- LGBT Patient Services & Support
- Transgender Patient Services & Support
- Patient Self Identification
- Medical Decision Making
- Employee Benefits and Policies
- Community Engagement
LGBT
patients and families are looking to this published index more and more to seek
out health care facilities and by extension their providers who can provide
LGBT culturally competent care. Facilities that rank the highest receive the
designation of Leader in LGBT Healthcare Equality which sets them apart from other
facilities/providers.
How do we go about achieving LGBT
cultural competence? Better
yet the question might be asked, how do we go about striving for LGBT Cultural Proficiency? Cross, et al
describes cultural proficiency: when
cultural differences are highly regarded and the need for research on
cultural differences and the development of new approaches to enhance
culturally competent practices are recognized. This level of achievement goes
beyond cultural competence: when cultural differences are accepted and
respected; continuous expansion of cultural knowledge and resources and
continuous adaptation of services occur; continuous self-assessment about
culture and vigilance toward the dynamics of cultural differences exist.
Achieving cultural competence and perhaps cultural proficiency
is a developmental process. First you have to recognize the need for doing
things differently, that you may not have all the answers. Secondly, you need
to determine who the key stakeholders are in making needed changes to policies
and procedures. Thirdly, you need the buy-in and active engagement of
leadership so that there is impetus behind the transformation. Lastly I would
say you need to actively involve the LGBT community in assessing current state,
what needs to change, what can change and to provide the motivation for making
the changes.
Delaware’s largest private employer, Christiana Care Health System,
has been participating in the Healthcare Equality Index since 2011 and since
2012 the system’s two hospitals: Christiana Care Wilmington Hospital and
Christiana Care Christiana Hospital have received the designation of Leader
in LGBT Healthcare Equality. All new nurses hired by the system receive
comprehensive orientation. During the orientation day titled “Exceptional
Experience” they participate in an education module called Your LGBTQ Patient: Providing Culturally Competent Care.
The
strategies employed in this education module with additional resources will be
presented in the Train-the-Trainer Webinar that Tim Rodden, MDiv, MA, BCC,
FACHE and Bret Herb, LCSW will conduct on June 16, 2016 for the Association for
Nursing Professional Development. (Tim coordinates LGBT health for Christiana
Care and Brett is a gender therapist and mental health consultant for
Christiana Care.)


No comments:
Post a Comment